
Cancer treatment often involves multiple options based on general data about how most patients will respond to therapy. However, this approach may not be effective for everyone, as treatment responses and side effects can differ. As cancer therapies continue to advance and improve long-term survival rates, tailoring care to each patient’s specific needs becomes increasingly important.
How is cancer treatment selected today?
Typically, a cancer diagnosis presents a patient with several treatment options that have similar outcomes. These choices are based on research that estimates how people generally respond to the treatments and the side effects that they might experience. In other words, your doctor is relying on clinical studies that show similar results for most patients. But what if you’re not among those who benefit, or worse, are at risk of being harmed by the treatment?
Why and how can we tailor cancer treatments to individuals?
Tumor-specific biomarkers, such as HER2, EGFR, and estrogen receptor (ER), help doctors select the most appropriate treatment for a patient.1 Although these biomarkers have greatly enhanced cancer care, they have certain limitations. For instance, they do not predict how an individual patient will respond to treatment or what side effects they may experience.
Recent advances in genetics allow us to predict treatment side effects by analyzing the patient’s DNA, not just a tumor’s. By tailoring treatments in this way, doctors can strike the right balance between effective cures and minimizing harmful side effects to preserve quality of life. One area where personalized treatment is making notable progress is in prostate cancer.
Personalization of prostate cancer treatment
Most men with prostate cancer live long after diagnosis, with 95% thriving ten years later.2 While treatments like radiation therapy and surgery offer similar cure rates, they often come with long-lasting side effects.3 One of the most problematic is late genitourinary (GU) toxicity, which includes symptoms such as urinary tract pain, hematuria (blood in the urine), more frequent urination, and urinary urgency or leaking. These ongoing issues can require continuous medical care and seriously impact daily life. That’s why choosing the safest treatment is so important—it helps ensure the best possible quality of life so patients can focus on living well after their treatment, rather than being cured but having ongoing struggles with side effects.
What are the current choices in radiation therapy?
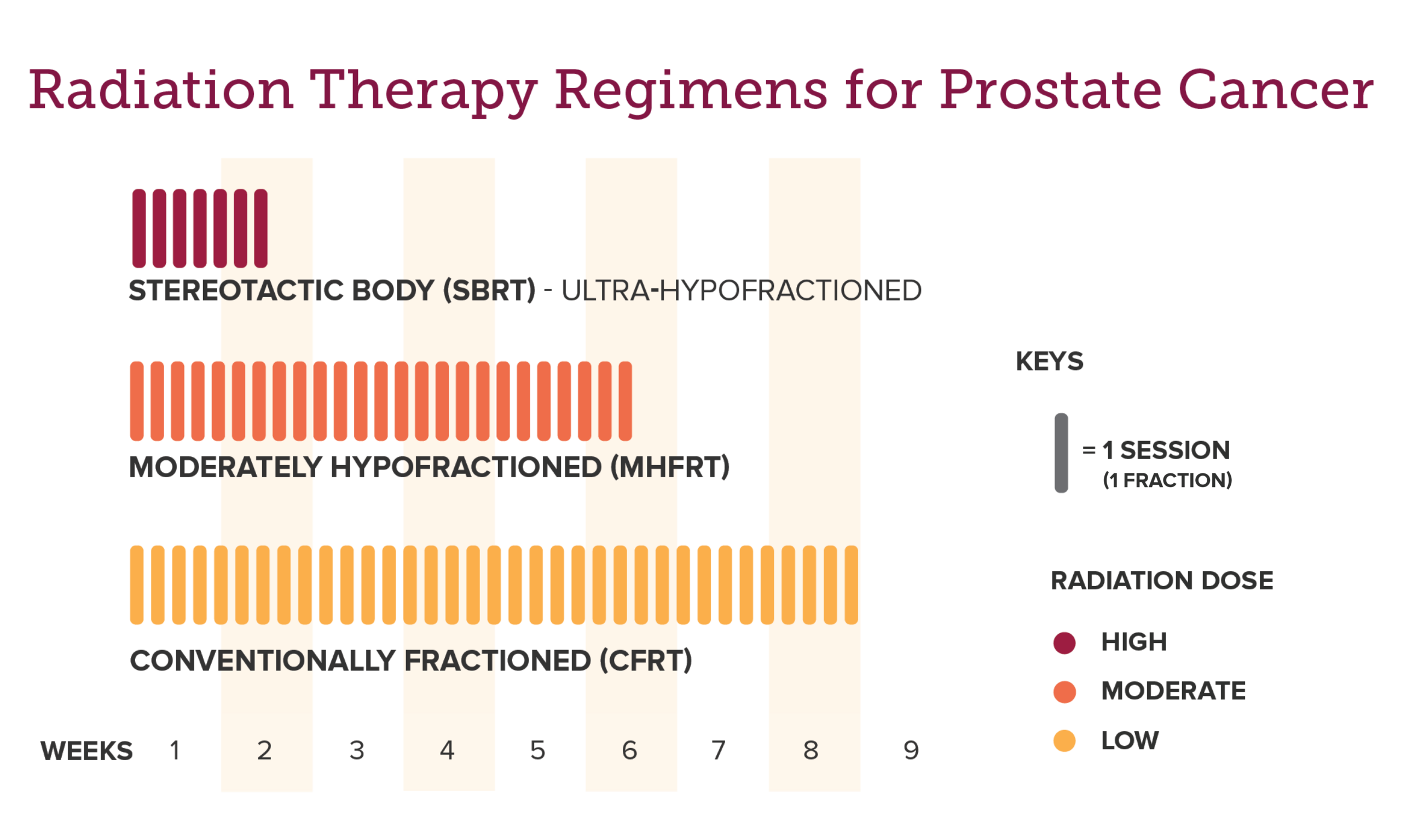
Prostate cancer patients can choose between ultra-fractionated radiation (SBRT) and more traditional methods, such as moderately hypofractionated radiation (MHFRT) or conventionally fractionated radiation (CFRT). While all three treatments deliver approximately the same total dose of radiation, they differ in the dose per visit and the duration of the entire treatment course.
The three most common radiation fractionation schedules are as follows:4
- SBRT (~5–7 high radiation doses over 5–10 days)
- MHFRT (~20–25 medium radiation doses over 4–5 weeks)
- CFRT (~35–45 low radiation doses over 8–10 weeks)
But the risk of late toxicity from each of these treatments can be quite different for an individual, highlighting the challenge and importance of personalized medicine. By assessing genetic biomarkers—measurable DNA sequences—doctors can now predict individual risks for side effects from a specific treatment, allowing them to help choose the safest option for the patient.
How do genetic biomarkers predict treatment risk?
The shift toward personalized cancer therapy, focused on safety and efficacy, is driven by groundbreaking research that has identified personal genetic biomarkers capable of predicting the risk of radiation toxicity.5 Dr. Weidhaas and colleagues have discovered specific genetic markers that can help identify individuals at risk of experiencing late GU toxicity from specific radiation treatments.6 What’s particularly exciting is that each person has a unique set of biomarkers that predict their risk of late GU toxicity, which is based on the type of radiation they receive.
For example, the PROSTOX ultra test identifies biomarkers associated with toxicity from SBRT, while the PROSTOX CFRT test identifies biomarkers linked to toxicity from CFRT. Since the biomarkers for each test are unique, a patient could be found to be at high risk of toxicity for one type of treatment but not for the other.
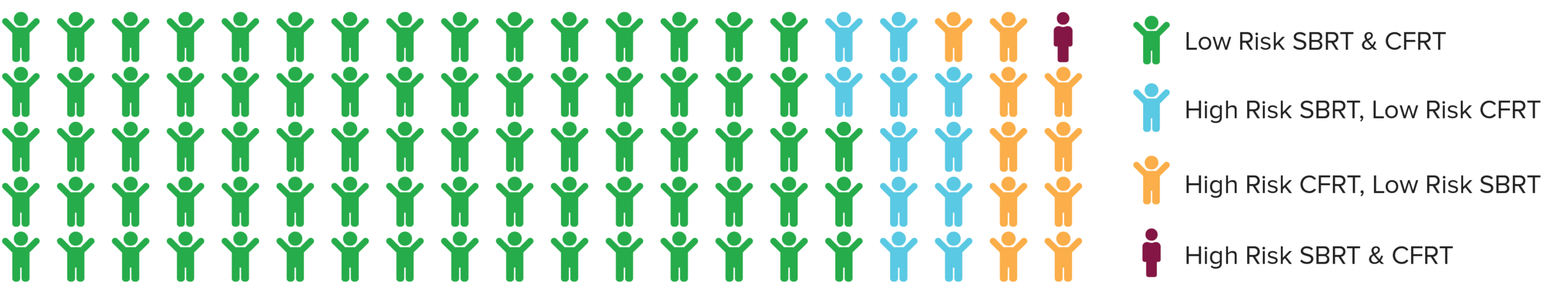
This means patients who are at high risk of toxicity may still be eligible for radiation therapy using a different, safer method tailored to their genetic profile. In the rare case when a patient is found to be at high risk of toxicity from both SBRT and CFRT (only 1%–2% of patients), alternative treatments are available and should be discussed with a doctor.
What does the discovery of these biomarkers mean for prostate cancer patients?
Imagine you’re going on a road trip, but you’re not sure which route to take. You could guess and see where the journey leads, or you could use GPS to find the most direct and efficient path. However, people like to see different things along the way and don’t always follow the same path. In the same way, PROSTOX testing helps you and your doctors “map out” the safest and best treatment options for your journey, tailored to you. By looking at your unique genetic biomarkers, these tests can predict the risk of toxicity for specific radiation treatments. If the results show a high risk for SBRT, you still have other radiation options, like CFRT. Similarly, the situation can also be reversed. Ultimately, it’s about making sure your treatment is as focused and personalized as possible, just like choosing the best route on a map.
Learn about PROSTOX and how it can help make your path to a better treatment plan possible.
Pioneering a new era in cancer treatment
PROSTOX testing is helping map out the best possible path for personalized prostate cancer treatment. Using this approach, a patient’s unique genetic biomarkers can help avoid detours caused by side effects and ensure the journey toward recovery is as smooth and direct as possible. And this is only the beginning. With ongoing research into other therapies, such as immunotherapy, we’re discovering even more genetic biomarkers that can refine treatment plans across different types of cancer, ensuring patients remain on the safest treatment path. Stay informed; subscribe to our newsletter for the most up-to-date research and tests.
Sharing hope and support for prostate cancer patients
If you know someone who has been diagnosed with prostate cancer, whether a loved one or a friend, please share this blog with them.
References
- https://www.nature.com/articles/s41392-024-01823-2
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/prostate-cancer-prognosis
- https://www.cancer.org/cancer/types/prostate-cancer/treating/considering-options.html
- https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/external-beam
- https://aacrjournals.org/cancerres/article/68/20/8535/541399/A-SNP-in-a-let-7-microRNA-Complementary-Site-in
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8979583/




Leave a Reply