Did you know that 80% of people affected by autoimmune diseases are women? This stark gender difference raises an important question: why are women more likely to develop autoimmune diseases than men? Research points to estrogen, and perhaps its fluctuations, as a key factor in this increased susceptibility.
In this blog, we’ll explore how estrogen impacts immune function, its connection to autoimmune diseases, how it may heighten the risk of these conditions, and strategies for managing them.
The Power of Estrogen: More Than Just a Reproductive Hormone
While estrogen is best known for regulating the reproductive system, its effects extend well beyond that. Estrogen is also necessary for maintaining healthy bones, heart, brain, and skin. Additionally, this hormone plays a major role in the immune system’s function.
How Estrogen Modulates the Immune System
Although we know that estrogen impacts the immune system, its effects are complex and not always clear-cut. In this section, we will explore the current understanding of how estrogen influences immunity.
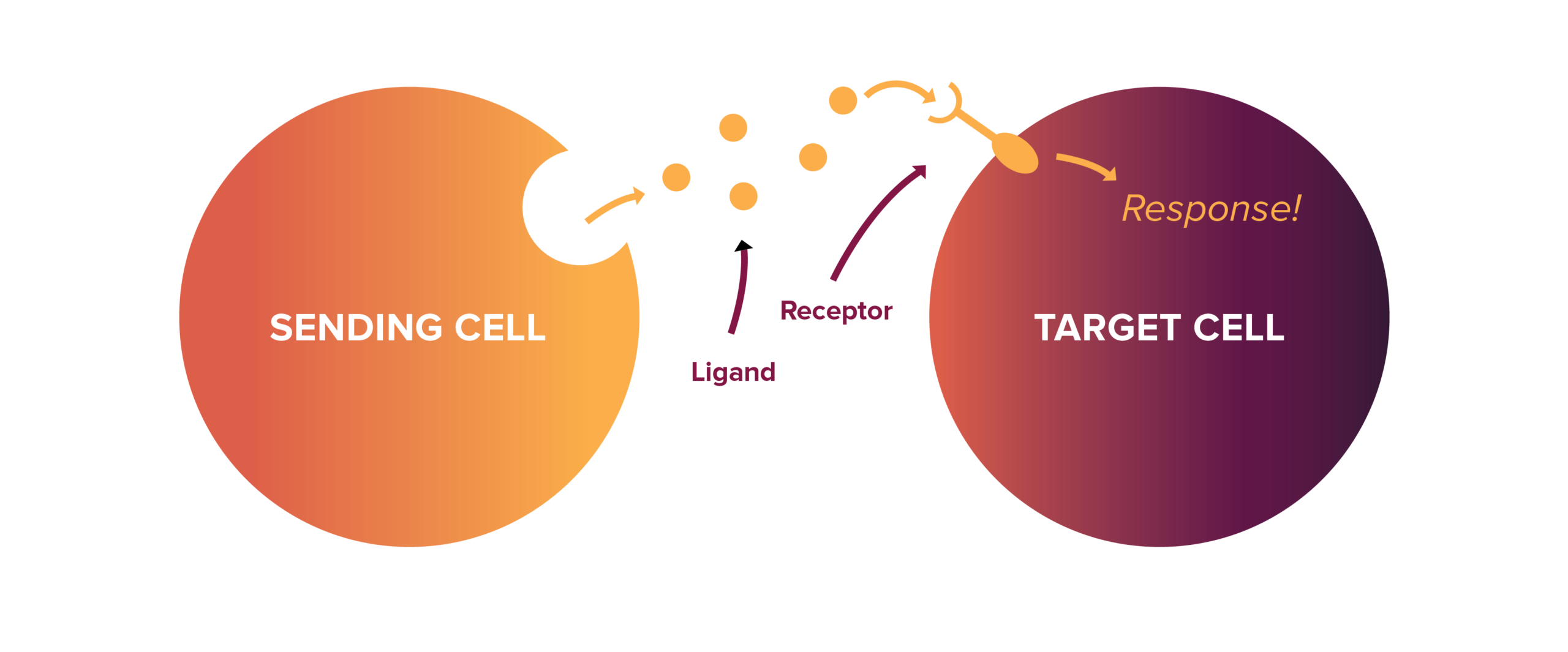
Cell Signaling — Interestingly, nearly all immune cells possess estrogen receptors, which function as locks, requiring the hormone estrogen as a “key” to trigger a response.1
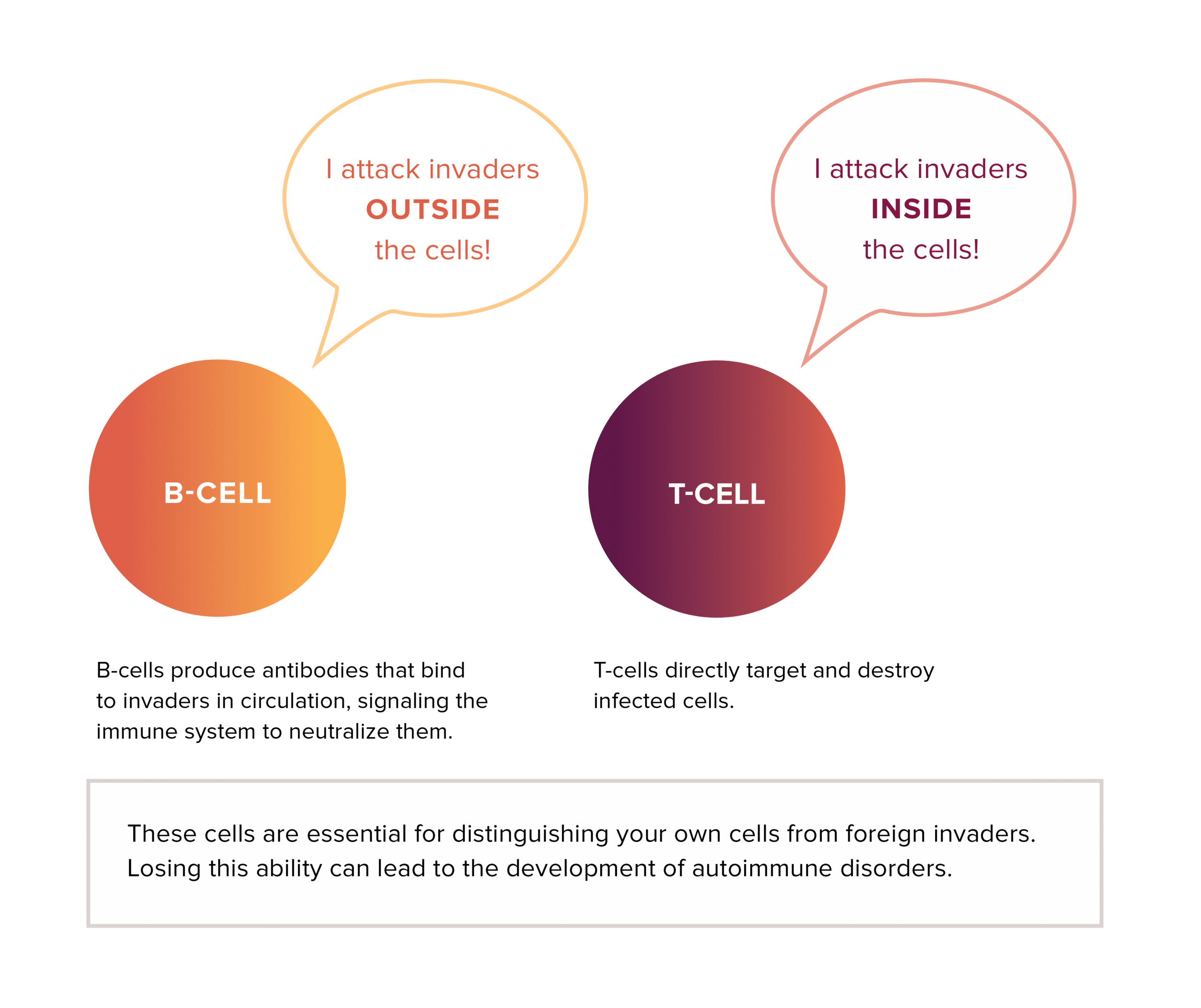
Cell Regulation — Estrogen helps activate immune cells, such as T-cells2-5 and B-cells6,7, to fight infections or respond to invaders. Without estrogen, these cells might not perform as effectively, leading to immune imbalance.
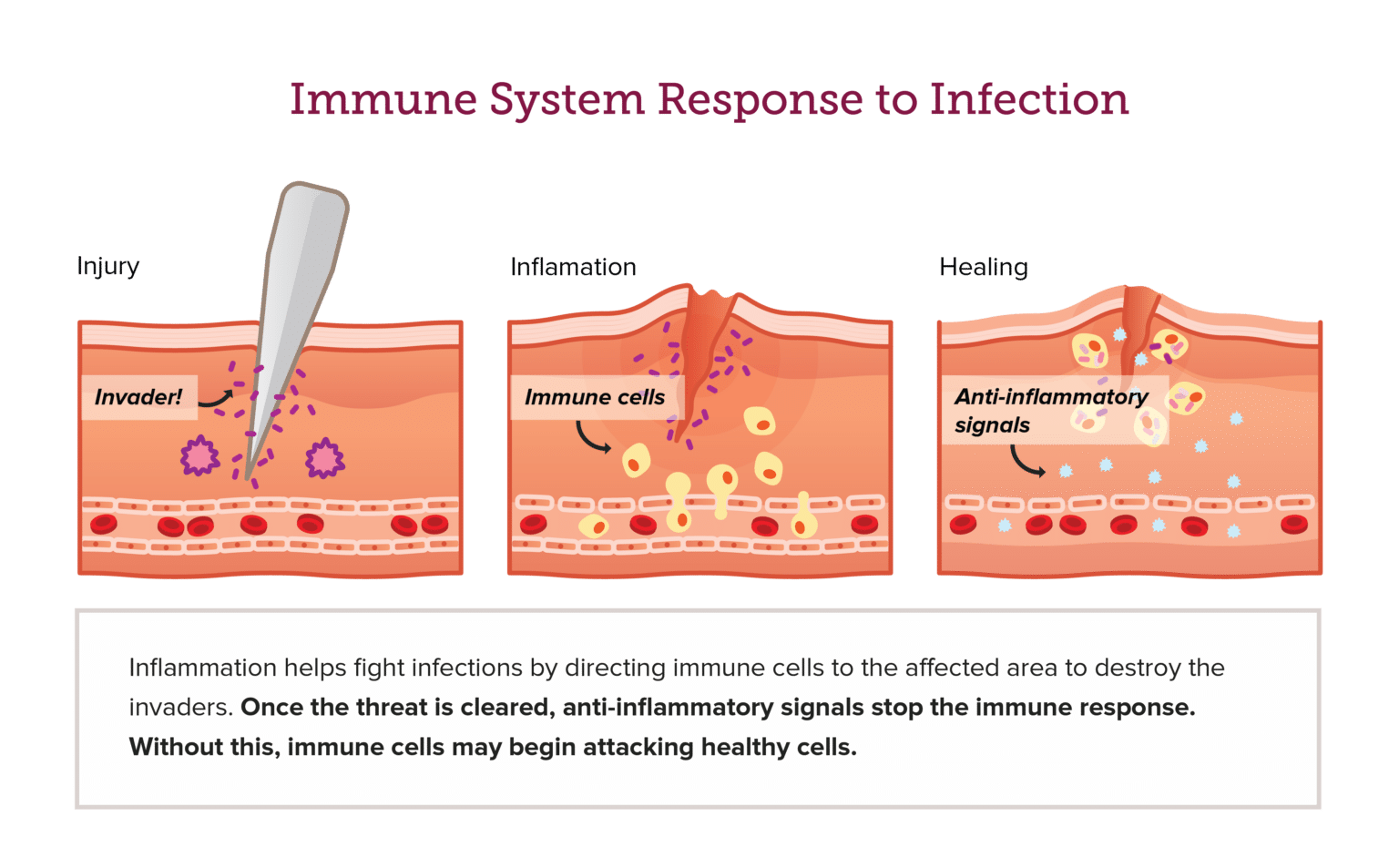
Anti-inflammatory Properties — Estrogen is generally recognized for its anti-inflammatory properties, which enable it to modulate immune cells and help control inflammation—a key aspect of the body’s response to infections.8-10
Understanding Autoimmunity: Why Your Immune System Can Go Rogue
Autoimmunity happens when the immune system, which is supposed to protect the body from harmful invaders like viruses and bacteria, mistakenly attacks its own tissues.11 This occurs when the immune system’s response becomes unbalanced—either lasting too long without being turned off or becoming too strong without the proper regulation.12-14 These errors can lead to chronic inflammation and damage to organs and tissues, which in turn can cause various autoimmune diseases.
Estrogen and Gender Differences in Autoimmune Disease Prevalence
In the mid-20th century, some of the first studies revealed that autoimmune diseases may be more prevalent in women than men.15,16 Today, it is known that approximately 80% of those affected by these diseases are women.17 One might wonder why this is the case. Unfortunately, the exact reason remains unclear, as autoimmune diseases are highly complex. However, since sex hormones interact with the immune system and estrogen fluctuates dramatically, one could hypothesize that some of these differences are due to this variability.
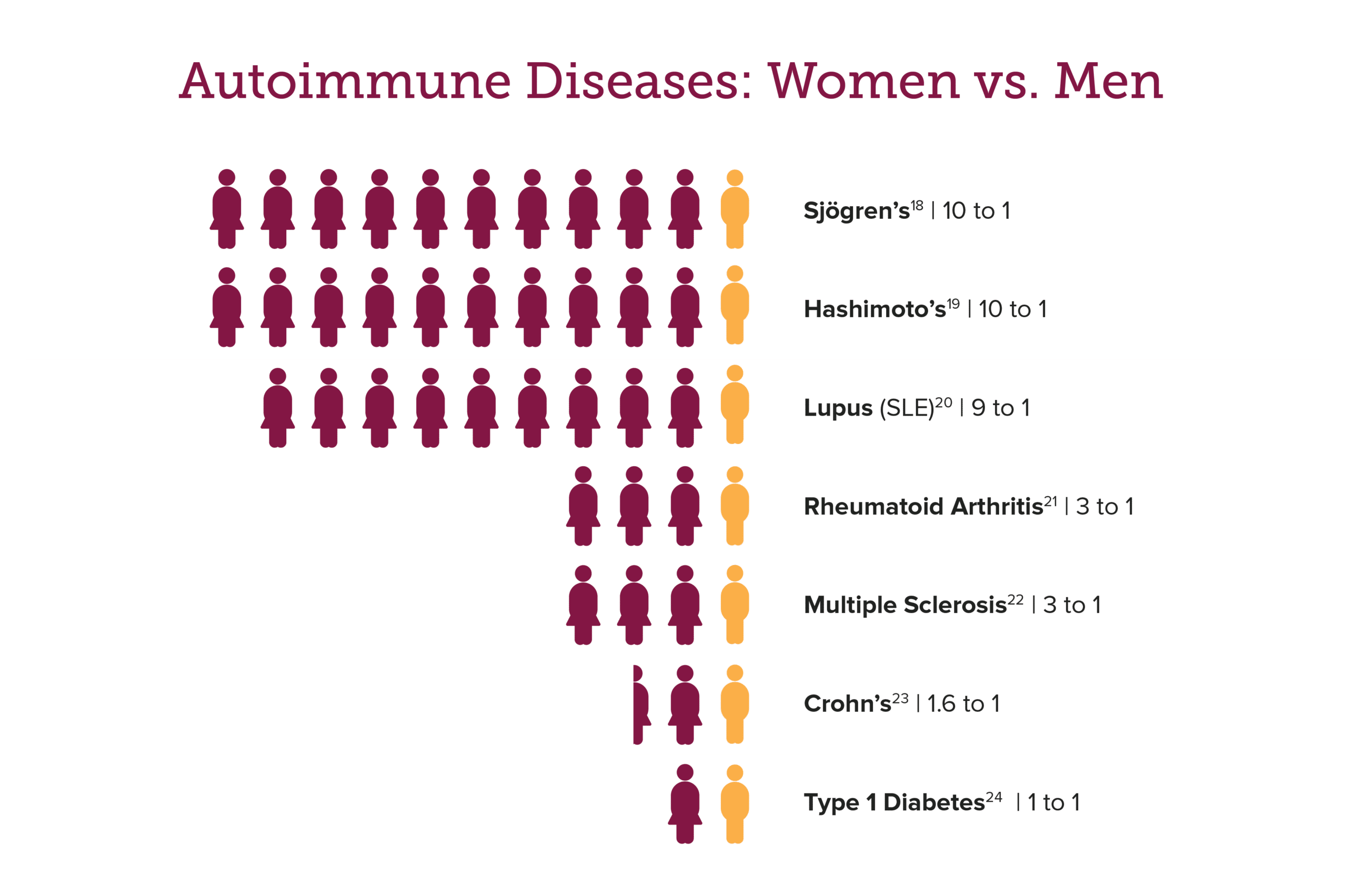
It’s important to note that not all women will develop an autoimmune disease. In fact, autoimmunity affects only 3.7% of women in the U.S.25 Experts believe a genetic predisposition and family history increase the risk for these women and that estrogen can act as a trigger.26 Estrogen can activate a stronger immune response, fluctuate throughout a woman’s life, and be influenced by certain medications, all of which may contribute to autoimmune conditions.
Estrogen’s Impact on Immune System Function and Autoimmune Risks
Higher estrogen levels are thought to strengthen the immune system in women, as compared to men. Research suggests that men are more vulnerable to illness, often experiencing more severe symptoms, while women typically exhibit stronger immune responses and recover from infections more effectively.27-30
While a stronger immune response helps protect against illness, it can also increase the risk of autoimmune diseases. Research indicates that viral infections triggering a strong immune response may contribute to the development of rheumatoid arthritis (RA) and multiple sclerosis (MS).31,32
Fluctuating Estrogen and Autoimmune Risks Throughout Life Stages
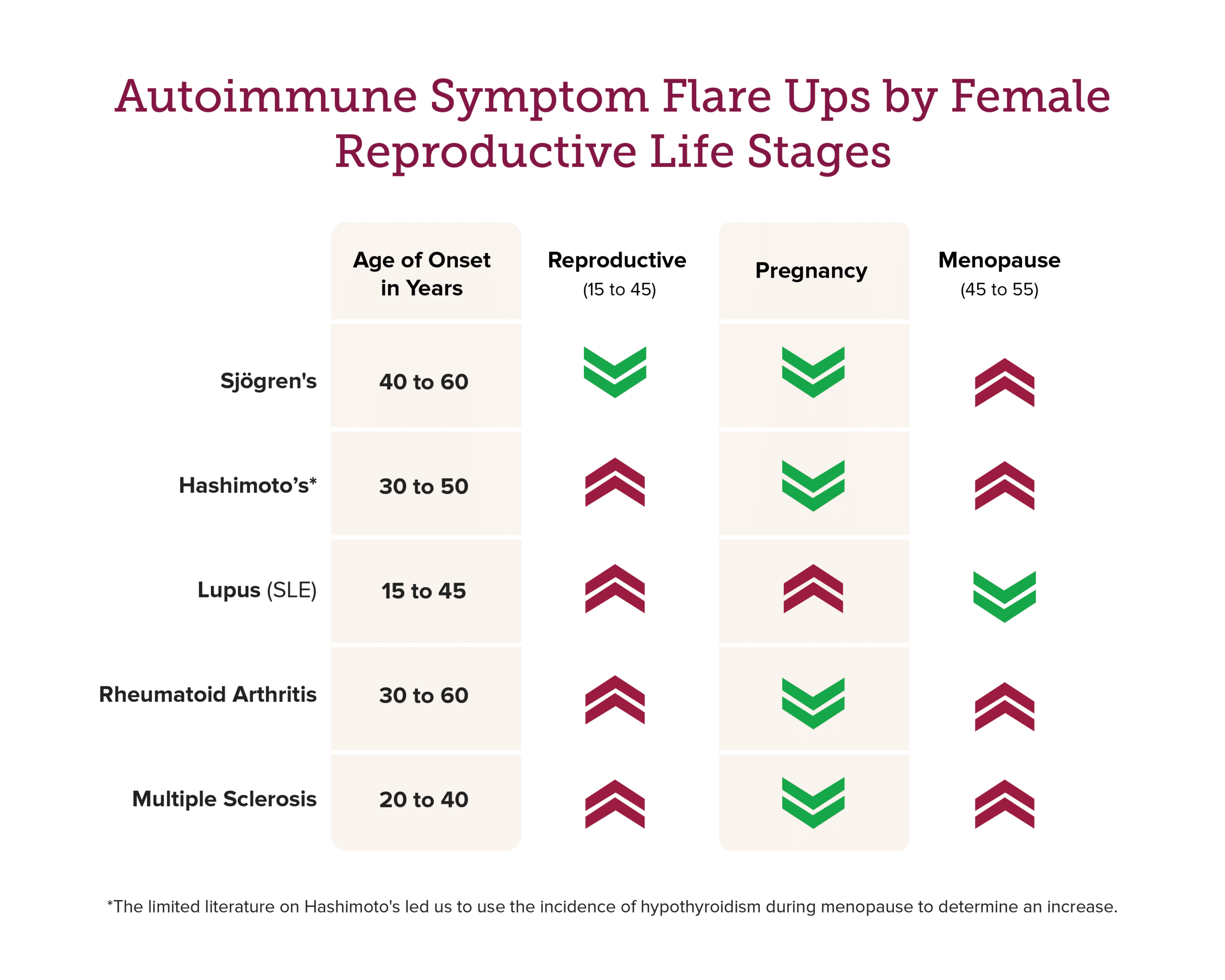
A woman’s susceptibility to autoimmune diseases can occur at any age, but they are commonly observed during two key life stages: a woman’s reproductive years and the menopause/postmenopausal years. During these periods, estrogen levels undergo significant fluctuations, which can influence preexisting conditions as well, supporting the hypothesis that changes in estrogen might be the culprit for elevated autoimmune diseases.
Reproductive Years
Fluctuating estrogen levels during the reproductive years can affect immune function, often making the immune system more active.33-37 These changes may increase susceptibility to autoimmune diseases, such as systemic lupus erythematosus (SLE)38, RA39, MS40, and Hashimoto’s thyroiditis (HT)41, especially in response to hormonal shifts during menstruation, pregnancy, and childbirth.
Pregnancy
During pregnancy, when estrogen levels peak, some autoimmune conditions may worsen. For example, women with SLE may experience flare-ups due to increased B-cell activity (your antibody-producing cells).42 Conversely, other conditions like RA and MS may improve, as elevated estrogen creates a more anti-inflammatory environment.43,44
Menopause
As women approach menopause and estrogen levels decline, the immune system can be affected, potentially triggering new autoimmune diseases or worsening existing ones. For example, reduced estrogen levels can weaken the body’s anti-inflammatory response, contributing to conditions like Sjögren’s syndrome and aggravating RA symptoms.45-48 MS and HT may also experience a second peak in incidence during menopause. However, overlapping symptoms with menopause can complicate diagnosis.49-51 On the other hand, women with SLE may actually find relief, as the drop in estrogen reduces its stimulating effects on the immune system.52,53
Impact of Hormone Therapies on Autoimmune Disease Risk
Estrogen’s impact on autoimmune conditions is multifaceted, with both its reduction and restoration affecting the immune system in different ways. Treatments that alter estrogen levels, like anti-estrogens and menopausal hormone therapy (MHT), formerly hormone replacement therapy (HRT), can have varied effects on women with autoimmune disorders.
- Anti-estrogens—Medications that block estrogen from binding to its receptors, like selective estrogen receptor modulators (SERMs), such as tamoxifen, and aromatase inhibitors (AIs), like anastrozole, are commonly used to treat hormone-sensitive breast cancer and other estrogen-related conditions. However, these treatments have been found to increase the risk of developing SLE and RA by reducing estrogen’s regulatory role on the immune system.59,60
- MHT—Hormone supplements can offer relief of menopause symptoms by restoring estrogen levels, but its effects can differ for women with autoimmune conditions. While some may experience symptom improvements, others may not. For example, MHT may increase the risk of developing SLE, but it doesn’t seem to worsen flare-ups. On the other hand, MHT may improve RA symptoms.61 It’s important to consider the potential benefits and risks of MHT and discuss them with your healthcare provider.
Managing Autoimmune Symptoms
Sadly, there is no cure for autoimmune disorders. Yet, there are ways to reduce risk and manage symptoms. Here are some strategies to consider:
- Medications—Autoimmune diseases require different treatments depending on the specific condition. Since each person’s immune system, genetics, and environment are unique, the type of treatment you need will depend on your specific condition. For example, women with HT may need medication to manage hypothyroidism. It’s important to consult a physician to determine the best treatment plan for you.
- Lifestyle Changes—In addition to medications, lifestyle changes can play a significant role in managing autoimmune symptoms. Adopting an anti-inflammatory diet, engaging in regular exercise, quitting smoking, and incorporating stress-reduction practices like yoga or meditation can help lower inflammation and support overall immune health.62-66
- Regular Check-ups and Monitoring—It’s important to monitor your autoimmune symptoms. Regular check-ups with your doctor can help catch any changes early. If you notice that your symptoms are worsening, discuss them with your healthcare provider to ensure your condition is managed effectively.
Estrogen plays a vital role in maintaining proper immune function, which is why women are more prone to developing autoimmune diseases than men. However, estrogen’s influence is not always predictable—its effects can vary greatly depending on a woman’s life stage and health history. By understanding these hormonal fluctuations and their impact on the immune system, women can take steps to manage their autoimmune health effectively.
If you’re experiencing new or worsening autoimmune symptoms, don’t hesitate to reach out to your doctor. By staying informed about how estrogen impacts health, women can better navigate their autoimmune risks and take proactive steps toward maintaining their well-being.
References
- https://anatomypubs.onlinelibrary.wiley.com/doi/10.1002/ar.24612
- https://pubmed.ncbi.nlm.nih.gov/15294932/
- https://onlinelibrary.wiley.com/doi/10.1002/jcp.21221
- https://pubmed.ncbi.nlm.nih.gov/16253347/
- https://pubmed.ncbi.nlm.nih.gov/30755659/
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1385501/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6626024/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2630539/
- https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-020-01998-9
- https://www.nature.com/articles/srep15224
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/autoimmune-disease
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8015752/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4870238/
- https://pubmed.ncbi.nlm.nih.gov/22029983/
- https://www.nature.com/articles/2141224a0
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1579130/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7292717/
- https://sjogrens.org/blog/2024/highlighting-men-with-sjogrens-disease-a-rheumatologists-perspective
- https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.00611/full
- https://rheumatology.org/patient-blog/differences-between-the-sexes-in-rheumatic-disease
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8537319/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9958616/
- https://link.springer.com/article/10.1007/s00592-022-02023-6
- https://newsnetwork.mayoclinic.org/discussion/new-study-calculates-autoimmune-disease-prevalence-in-u-s/
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.02279/full
- https://pubmed.ncbi.nlm.nih.gov/22101690/
- https://pubmed.ncbi.nlm.nih.gov/25278153/
- https://pubmed.ncbi.nlm.nih.gov/27546235/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5994698/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6754408/
- https://pubmed.ncbi.nlm.nih.gov/28963611/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6716891/
- https://pubmed.ncbi.nlm.nih.gov/21212088/
- https://www.science.org/doi/10.1126/scisignal.aap9415
- https://journals.aai.org/jimmunol/article/171/12/6936/72092/Estrogen-Receptor-Mediates-Estrogen-s-Immune
- https://rupress.org/jem/article/206/1/99/54186/Estrogen-directly-activates-AID-transcription-and
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2015.00635/full
- https://onlinelibrary.wiley.com/doi/10.1155/2014/615917
- https://pubmed.ncbi.nlm.nih.gov/17393454/
- https://bmcrheumatol.biomedcentral.com/articles/10.1186/s41927-024-00429-z
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7772117/
- https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/symptoms-causes/syc-20351855
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1233883/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5722767/
- https://academic.oup.com/rheumatology/article/50/11/1955/1787741
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4630965/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9884461/
- https://pubmed.ncbi.nlm.nih.gov/24101131/
- https://my.clevelandclinic.org/health/diseases/12120-hypothyroidism
- https://pubmed.ncbi.nlm.nih.gov/22120060/
- https://www.sciencedirect.com/science/article/abs/pii/S1568997211002680?via%3Dihub
- https://www.mayoclinic.org/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
- https://my.clevelandclinic.org/health/diseases/17665-hashimotos-disease
- https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789
- https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
- https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis
- https://www.jrheum.org/content/42/1/55.long
- https://www.sciencedirect.com/science/article/abs/pii/S1568997220300112
- https://www.tandfonline.com/doi/full/10.1080/13697130903025449
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8620243/
- https://www.autoimmuneinstitute.org/articles/culinary-medicine-autoimmunity-and-healthful-eating/
- https://www.sciencedirect.com/science/article/pii/S209525462400019X?via%3Dihub
- https://www.jhep-reports.eu/article/S2589-5559(22)00022-2/fulltext
- https://pubmed.ncbi.nlm.nih.gov/26772647/




Leave a Reply