
Heart disease is the leading cause of death for women in the United States. While it can affect women at any age, it increases after menopause. In part, this is due to the decrease in estrogen, which provides protection against heart disease in premenopause. So why not replace estrogen? You may have already heard about menopausal hormone therapy (MHT), formerly hormone replacement therapy (HRT), a method of replacing estrogen, but have heard positives and negatives. The history of MHT has been complex, filled with information that might have left you feeling confused. Our goal at MiraKind is to help clear the clutter and provide you with accurate information regarding MHT and its link to heart disease.
Heart disease
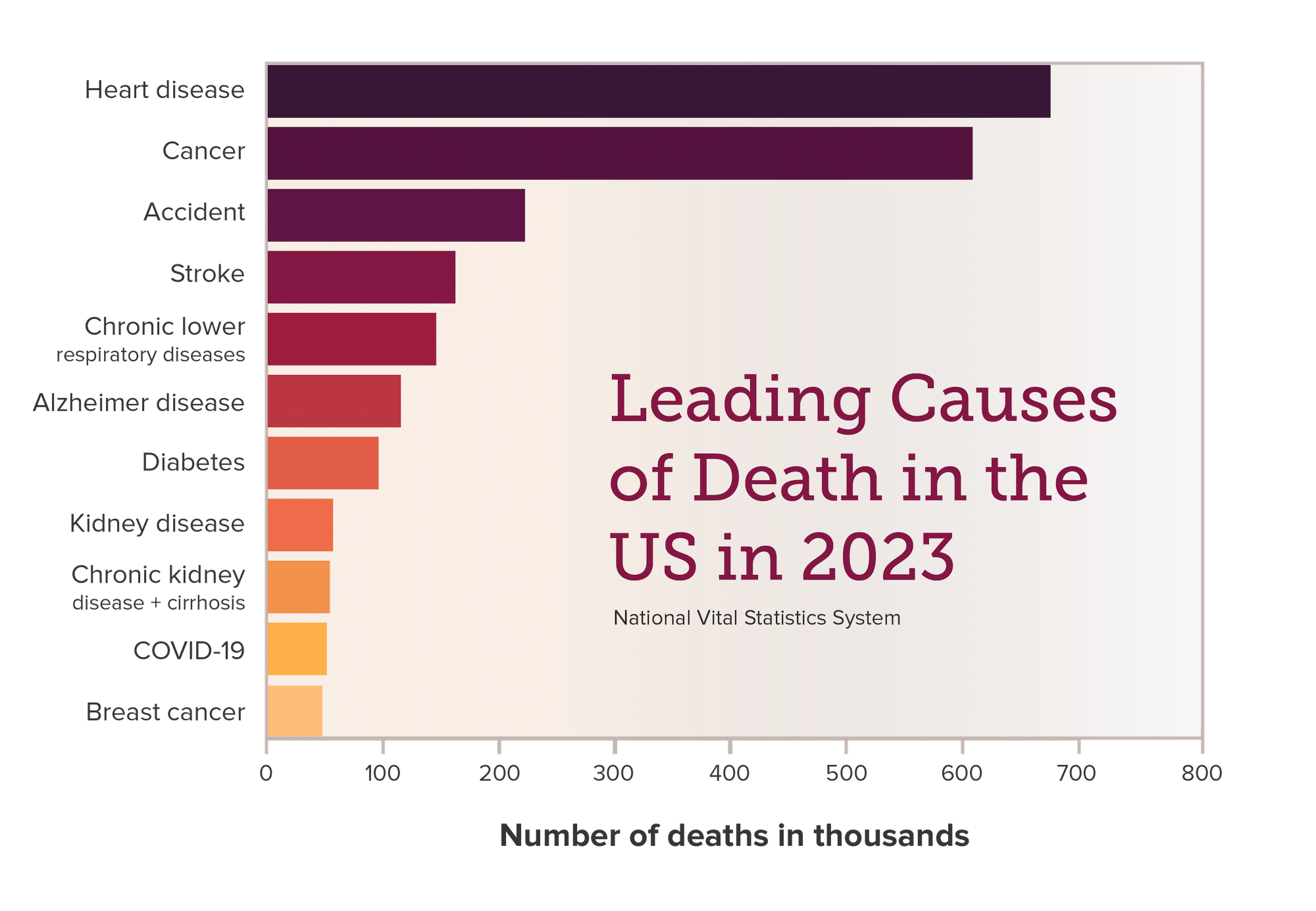
The term “heart disease” refers to several types of heart conditions. This includes coronary artery disease (CAD), arrhythmias, heart valve disease, cardiomyopathy, heart failure, congenital heart disease, and issues in the lining of the heart, to name a few.1 In 2023, heart disease was the leading cause of death in the US for both men and women, accounting for a total of 681,185 documented deaths, 305,036 of which were women.2
Women and Heart disease
Surprisingly, many women remain unaware of this danger. Surveys have shown that most women believe cancer, especially breast cancer, is the main cause of death. Yet, heart disease kills more women than all cancers combined.
How does estrogen protect against heart disease?
In women, estrogen plays an important role in breast development, menstrual cycles, ovulation, and more. However, estrogen has the potential to impact your health in many other positive ways.
In your premenopausal years, estrogen protects the heart by:
- Reducing scarring (fibrosis)
- Increasing blood flow
- Improving heart function
- Reducing free radicals (unstable molecules that can damage cells)
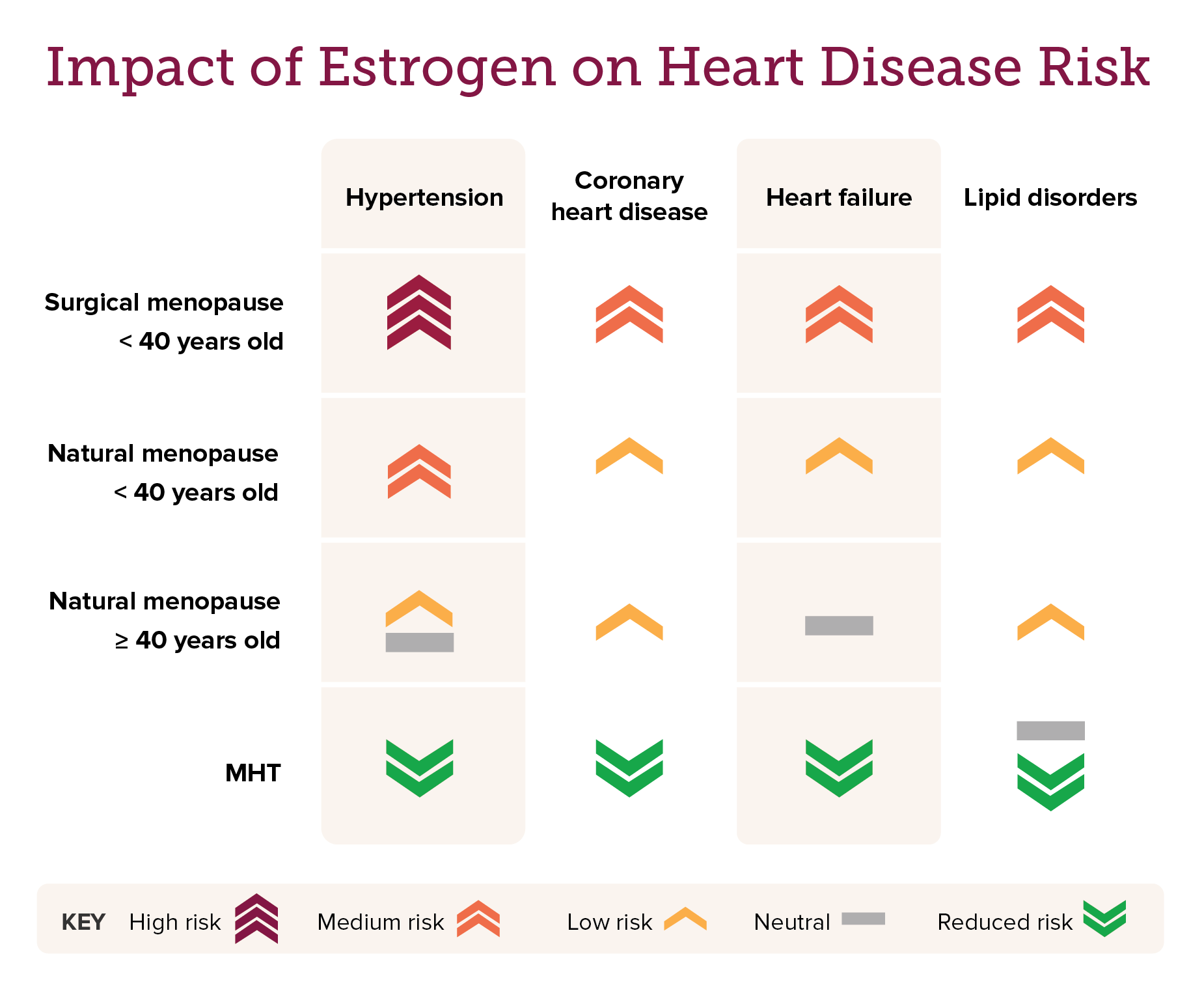
All of the above reduce your risk of heart disease.3 Women in menopause (and men too) are not protected as well from heart disease because they have lower estrogen levels.
MHT and heart disease
During the early to mid-20th century, medical observations revealed that women develop heart disease approximately ten years later than men. This timing appears to align with the start of menopause and a decrease in estrogen levels.4,5 For most women, a significant decline in estrogen triggers menopausal symptoms.
In 1942, the Food and Drug Administration (FDA) approved the first estrogen MHT for the effective treatment of menopausal symptoms, providing women relief from hot flashes, night sweats, and vaginal dryness. Interestingly, by the 1970s, observational studies began noting a decrease in heart disease in women when taking MHT. The accumulation of observational studies led to the first large-scale randomized clinical trial, the 1998 Women’s Health Initiative (WHI), that asked, “Does MHT prevent heart disease, cancer, and osteoporosis in postmenopausal women?”
The WHI MHT study: Two steps forward and a giant leap backward
The 1998 WHI trial enlisted approximately 68,000 women between the ages of 50 and 79 and divided them into two arms of the study: one arm received estrogen with progesterone and the other received estrogen alone.6 Each arm included a placebo group of equal participants who did not take MHT. Certain risks emerged in the MHT groups, causing concern and the decision to end the study early. The estrogen with progesterone arm reported an increased incidence of coronary heart disease and breast cancer, while the estrogen alone arm reported a small increased risk of stroke in the absence of other significant cardiovascular benefits.7,8
The release of the WHI results had an almost immediate negative impact on perceptions of MHT.
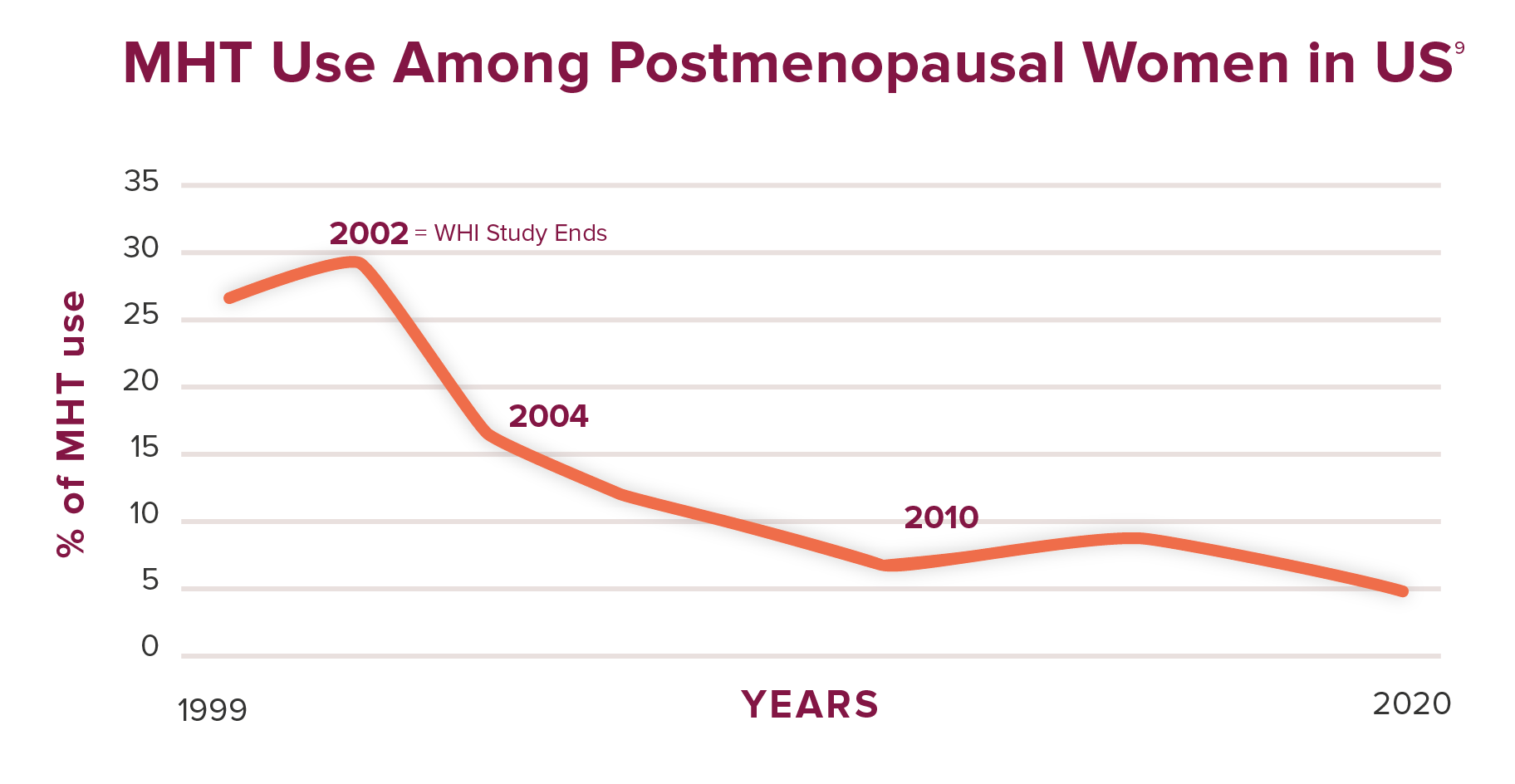
Many doctors stopped prescribing MHT, and many women abandoned it immediately, leading to a marked decline in its use. The effects have lasted to this day.
However, there were several major limitations to the WHI trials
The participants’ average age was 63 years, and there was no screening for preexisting heart disease. On average, women enter menopause at age 50, and the decline in estrogen causes them to be more susceptible to heart disease. We can presume that some women over 60, especially those who had not had MHT, might have had preexisting conditions for heart disease. What would the data look like if we removed these women?
Upon reanalysis of the data for women between the ages of 50 and 59, a favorable risk-benefit ratio was found; MHT reduced heart disease and all-cause mortality (death due to any cause).10
Another concurrent trial in Denmark further confirmed this data. This trial, with an average participant age of 50, found that healthy women who took estrogen with progesterone or estrogen alone for ten years after menopause had a lower risk of heart disease and heart disease-related deaths. Additionally, this trial found no increase in cancer, particularly breast cancer.11
However, the media’s reporting of the early findings of the WHI trial overshadowed this new information. The negative results of the initial study received wide publicity, creating panic among MHT users and prescribing physicians. The media’s clear message was that MHT posed more risks than benefits for all women.
Does MHT prevent heart disease in women? Where we stand today.
While the benefits and risks are still debated, current research has begun to support MHT use. Numerous studies have shown that women who lack estrogen, including its decline during menopause, have a higher risk of heart disease compared to those with normal estrogen levels.12,13 This finding creates a positive shift in the belief that estrogen can be beneficial. Moreover, studies have found that replacing estrogen in the form of MHT at the onset of menopause can reduce the risk of heart disease later in life for healthy women.14-16
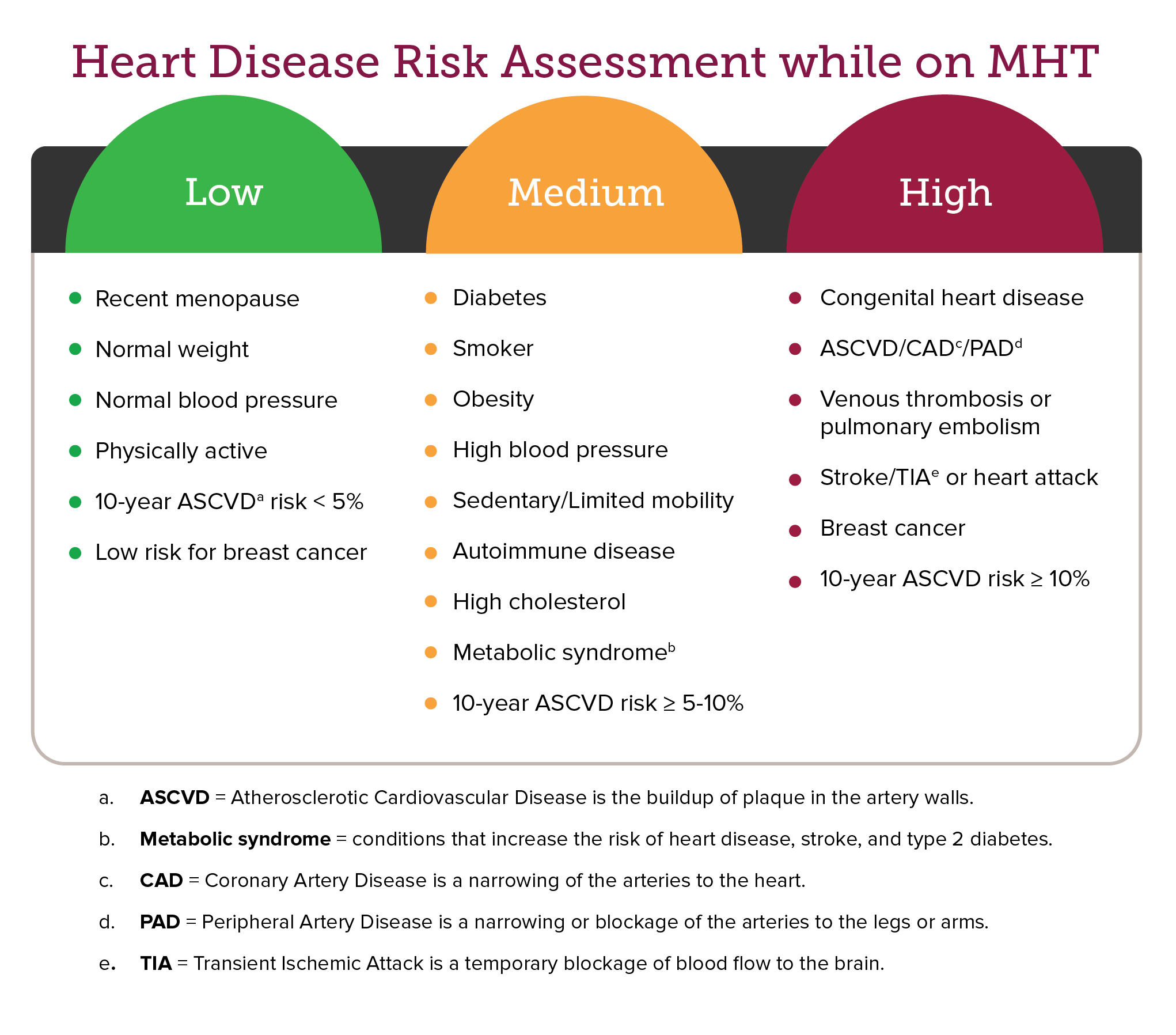
However, some women may be more prone to heart disease than others, and there are additional risk factors linked to MHT. Keep in mind that some studies, including the WHI, have shown that women over 60 who started taking MHT more than ten years after the onset of menopause do have a higher risk of heart disease. Besides age, other risk factors can increase the risk of heart disease. The following table provides guidelines for evaluating the risk of heart disease development while on MHT.17
Final takeaways on heart disease and MHT for women
As heart disease remains the number one killer of women, the option to take estrogen at the onset of menopause should be something to consider. However, taking MHT is a personal decision where one must weigh the risk against the benefits. The decision should consider numerous factors, including health and family history of disease, the severity of menopausal symptoms, age of menopause, etc. And you should not be alone in this decision. Speaking with a doctor who understands menopause, MHT, and the latest data can assist you in making an informed decision and monitor your response to MHT, if you choose to use it.
We are conducting a study about MHT and its impact on women’s health. Subscribe for our latest research updates!
Recommended Reading:
- Menopause & Myths about Menopausal Hormone Therapy
- Let’s learn more about Menopausal Hormone Therapy – together!
- Hormones, the KRAS-variant, and Breast Cancer Risk
- Recent Research on Estrogen and Alzheimer’s Disease
- Menopause and Mental Health
References
- https://my.clevelandclinic.org/health/diseases/24129-heart-disease
- https://wonder.cdc.gov/mcd.html
- https://doi.org/10.1186/s13293-017-0152-8
- https://pubmed.ncbi.nlm.nih.gov/29338561/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6734083/
- https://www-whi-org.s3.us-west-2.amazonaws.com/wp-content/uploads/Protocol-1993-2005.pdf
- https://jamanetwork.com/journals/jama/fullarticle/195120
- https://jamanetwork.com/journals/jama/fullarticle/198540
- https://jamanetwork.com/journals/jama-health-forum/fullarticle/2823976
- https://jamanetwork.com/journals/jama/fullarticle/206404
- https://www.bmj.com/content/345/bmj.e6409.long
- https://pubmed.ncbi.nlm.nih.gov/28923176/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9479724/
- https://journals.lww.com/menopausejournal/fulltext/2019/09000/the_kronos_early_estrogen_prevention_study.21.aspx
- https://www.acpjournals.org/doi/10.7326/M14-0353?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1484709/
- https://doi.org/10.1161/CIRCULATIONAHA.122.06155




Leave a Reply