
A new clinical trial published in the New England Journal of Medicine may change how some breast cancer patients are treated with radiation after chemotherapy and surgery. We spoke with Dr. Terry Mamounas, the study’s lead author and a respected breast cancer expert, to explore how this research may allow certain patients to safely avoid lymph node radiation, potentially sparing them unnecessary treatment and potential side effects.
In this blog, we summarize key insights from both the peer-reviewed publication and our in-depth conversation with Dr. Mamounas.
When Chemotherapy Clears Lymph Nodes, Is Radiation Still Needed?
Neoadjuvant chemotherapy is a strategy used for many breast cancer patients who require chemotherapy as part of their treatment plan. It is sometimes given before surgery to shrink tumors, making breast-conserving surgery, i.e., lumpectomy, possible instead of a mastectomy. Most importantly, it helps guide treatment decisions about whether additional chemotherapy is needed after surgery, particularly if the tumor remains.
Neoadjuvant chemotherapy is a cancer treatment given before surgery to help make the tumor easier to remove, guide further treatment decisions, and provide information on outcomes.
In many patients who receive neoadjuvant chemotherapy, breast cancer has spread to nearby lymph nodes. The standard has been for doctors to use radiation therapy after neoadjuvant chemotherapy and surgery to target all local lymph node areas.
As neoadjuvant chemotherapy becomes more common and effective, doctors are increasingly seeing patients who initially had cancer in their lymph nodes but, after treatment, have no remaining cancer found in the lymph nodes that were tested—a status called a pathologic complete response, or ypN0.
Growing data suggest that for these ypN0 patients, radiation to the remaining lymph nodes may not be necessary. This study was conducted to confirm just that.
Who Participated and What Was Tested
The NSABP B-51 trial that Dr. Mamounas led was a large, international study involving over 1,600 breast cancer patients from medical centers in the U.S., Canada, Japan, and other countries. The goal of the study was to see if radiation was necessary in patients who had neoadjuvant chemotherapy and were ypN0 in the sampled lymph nodes at the time of surgery (no cancer cells were left in the lymph nodes that were tested).
Once ypN0 status was confirmed, patients were randomly assigned to one of two treatment arms:
- Lymph node radiation
- No lymph node radiation
The researchers tracked treatment outcomes to determine whether radiation of the remaining lymph nodes prevented cancer from coming back—and whether it affected survival and recurrence.
Does Radiation to the Lymph Nodes Help If No Visible Cancer Remains After Chemo?
According to the study’s results, for many patients, the answer appears to be no.
After nearly five years of follow-up, there was no significant difference between the two arms in terms of breast cancer recurrence and survival. In fact, 92.7% of patients who received lymph node radiation remained free of invasive breast cancer, compared to 91.8% of those who did not receive it, regardless of demographic variables such as age, race, and ethnicity.
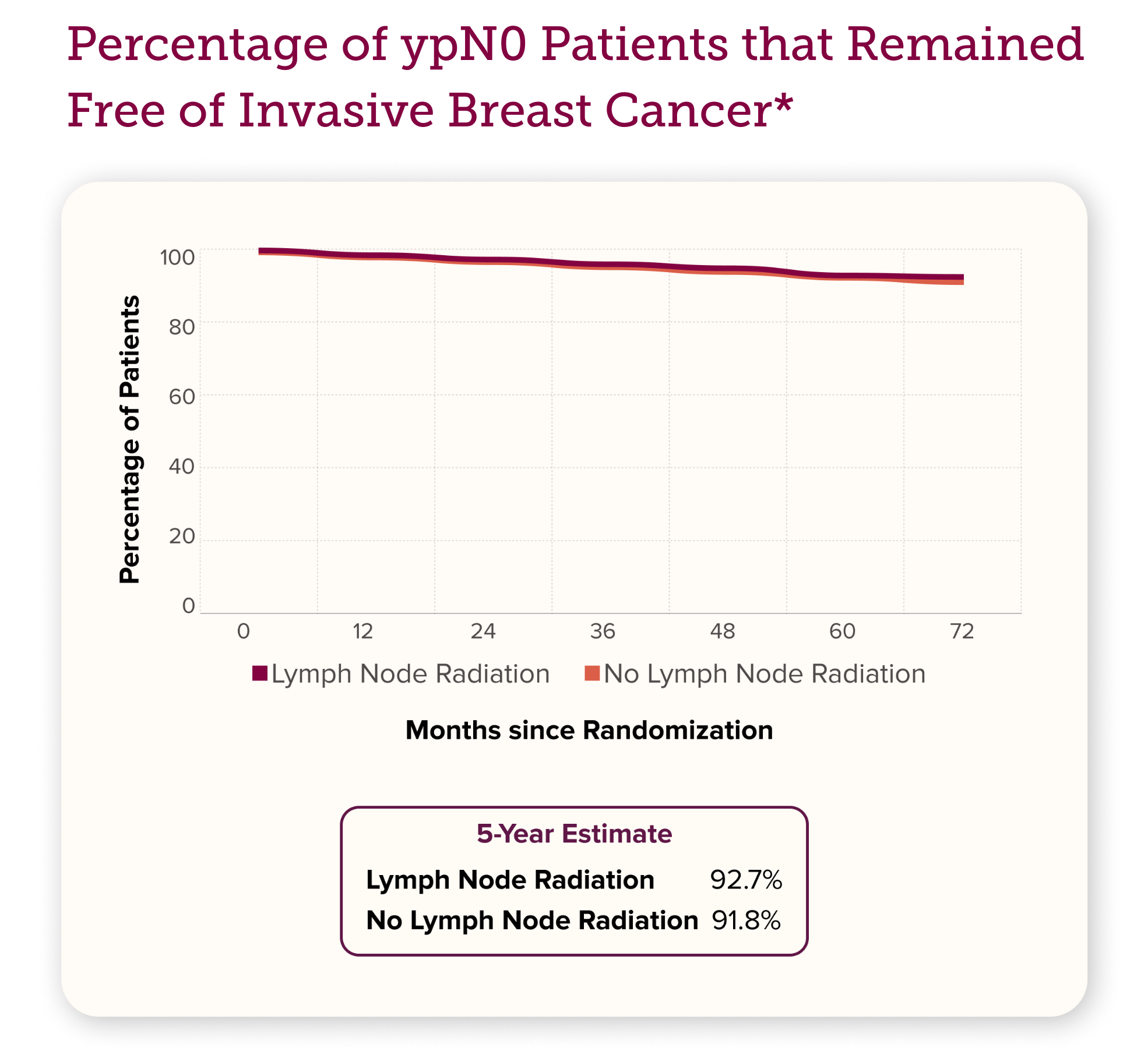
This finding—that the remaining lymph nodes didn’t need treatment after neoadjuvant chemotherapy when no cancer cells were found in lymph nodes tested at the time of surgery—appeared to be true across different types of breast cancer, including hormone receptor positive, HER2 positive, and triple negative.
Why This Study Could Change Breast Cancer Treatment
For patients diagnosed with lymph node–positive cancer who achieved ypN0 status after neoadjuvant chemotherapy, omitting lymph node radiation did not compromise outcomes. These findings support a paradigm shift toward personalized treatment plans that prioritize a patient’s response to therapy versus those based on the initial diagnosis alone.
Therefore, rather than recommending lymph node radiation for all breast cancer patients with node-positive disease at diagnosis—as is routine—oncologists may now consider withholding radiation to these areas in select cases based on how the cancer responds to chemotherapy.
What Does This Mean for Breast Cancer Patients?
For patients whose lymph nodes are clear after neoadjuvant chemotherapy (a pathologic complete response, or ypN0), this study suggests that some may safely avoid radiation to the remaining lymph nodes. This could lead to fewer hospital visits, reduced risk of side effects, and more energy for recovery. Still, radiation may be the right choice for some. Talk with your doctor to decide what is best for you.
Making Breast Cancer Treatment Safer and More Personal
While serious side effects from radiation to the breast are uncommon, they occurred more frequently in patients who received lymph node radiation. Therefore, avoiding unnecessary radiation to the lymph nodes could help reduce side effects and improve quality of life.
Some patients may still choose lymph node radiation as a precaution. But what if there was a way to identify those at higher risk for side effects in advance—helping to guide that decision?
At MiraKind, we’re studying inherited genetic variants in microRNAs, called mirSNPs, that may help predict who is more likely to experience side effects from radiation therapy.
In fact, MiraKind has discovered a specific mirSNP signature linked to breast cancer, which could help identify patients at greater risk of side effects from radiation therapy—before treatment begins. Our goal is to empower both doctors and patients with information so they can make safer, more informed treatment decisions.
Conclusion
This study offers encouraging news for many breast cancer patients: if neoadjuvant chemotherapy clears the cancer from the tested lymph nodes, it may be safe to avoid radiation to those remaining lymph node areas.
With continued research, including genetic studies like those here at MiraKind, the future of cancer care looks not only more precise but also more compassionate, giving patients the best chance at recovery with the least amount of harm.
Watch the full interview here.
Read the published study here.
Breast Cancer Treatment: Top FAQs About Lymph Node Radiation After Neoadjuvant Chemotherapy
Q: What is neoadjuvant chemotherapy for breast cancer?
A: Neoadjuvant chemotherapy is a treatment given before surgery. It can help make breast-conserving surgery possible and assess how well the cancer responds to chemotherapy to help guide additional treatment decisions.
Q: What does ypN0 mean in breast cancer treatment?
A: A ypN0 status refers to the absence of cancer in the lymph nodes tested after neoadjuvant chemotherapy, as confirmed at the time of surgery. It is a positive sign that the cancer has responded well to the chemotherapy treatment.
Q: Can breast cancer patients avoid lymph node radiation after chemotherapy?
A: According to a new study published in the New England Journal of Medicine, some breast cancer patients with ypN0 status after neoadjuvant chemotherapy may safely avoid lymph node radiation without affecting survival or recurrence rates.
Q: What are the risks of lymph node radiation therapy?
A: Lymph node radiation can increase the risk of side effects such as lymphedema (swelling in the arm).
Q: How do doctors decide if lymph node radiation is needed?
A: Historically, if cancer was found in the lymph nodes before chemotherapy, it was standard for patients to receive radiation therapy for those areas after completing both chemotherapy and surgery. However, this new study suggests that radiation may not be necessary in some cases—particularly if no cancer remains in the lymph nodes tested after chemotherapy at the time of surgery.
References
Mamounas EP, et al. Omitting Regional Nodal Irradiation after Response to Neoadjuvant Chemotherapy.N Engl J Med. 2025;392:2113-2124.




Leave a Reply