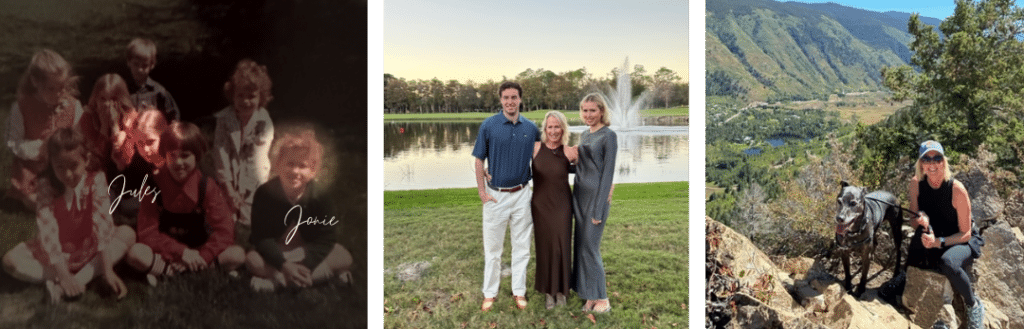
When Julie Hess and Dr. Joanne Weidhaas met as second graders in Michigan, it was the beginning of a lifelong friendship.
“I called her by her nickname, Jonie, and she called me Jules,” Julie remembered. “She’s a twin, and she and her brother and I were like siblings. We grew up together straight through high school.”
After graduation, Joanne left to earn her degree in biology at Yale, but the two reunited when Julie’s then-husband took a job in Boston at the same time that Joanne was earning her MD and PhD in Medicine at nearby Tufts University.
“We both had our first children just a few months apart while we were in Boston,” Julie said.
Even as life took them to different states, the two stayed in touch, so it wasn’t a surprise when Julie reached out to get Joanne‘s opinion on a medical matter a few years ago.
At the time, Julie was in her late 40s and going through menopause. The hot flashes, fatigue, and mental fogginess were so intense, that she was considering starting hormone replacement therapy.
“I lead a fairly natural and healthy lifestyle,” Julie said. “I’ve never taken medication long-term, so this was a pretty drastic decision for me, and I called Joanne to see what she thought about HRT.”
Joanne took her through the studies on HRT and cancer risk – the ones from the early 2000s that indicated an increased risk for breast cancer and blood clots with HRT and more recent ones that HRT is safer than previously believed and that the benefits generally outweighed the risks.
Joanne then suggested that her friend be tested for the KRAS-variant. Julie agreed and within a few days found out that she did in fact have the variant.
“It was definitely scary to receive that news,” Julie said. “For a while, I just sat with that information that I had tested positive.”
Julie’s mother also got tested and was positive for the KRAS-variant. Neither has been diagnosed with cancer, although other women on Julie’s maternal side did have cancer.
Joanne recommended that with this new knowledge, Julie should increase her screenings for both breast and ovarian cancer and continue to remain on HRT. Julie began a regimen of 6-month vaginal ultrasounds, along with alternating between a mammogram or an MRI every six months.
When one of the ultrasounds showed that Julie had large fibroids that were growing, she and her OB-GYN discussed her options, particularly in light of having the KRAS-variant. Ultimately, Julie opted to have a full hysterectomy, removing her uterus and ovaries.
“That decision wasn’t easy, but I could wrap my head around it,” she said.
It was tougher deciding what to do about her breasts. Prior to getting tested for the KRAS-variant, Julie had already had a breast biopsy because of a cancer concern. She was diagnosed with dense breasts, and she had gotten breast implants in 2015, which complicates mammogram readings. “I wouldn’t have done that if I had known about having the KRAS-variant,” she said.
On top of that, the schedule of having a mammogram and then an MRI six months later was leading to what is known as “scanxiety,” often a severe anxiety related to cancer screening tests, in part because of the machinery used for testing and in part because of the fear of negative news regarding the test results.
She began to lose sleep waiting for results, and then dreading when the next appointment would come up. She particularly hated the MRI exams, where she would spend 45 uncomfortable and loud minutes stuck in a tube.
Plus, it felt like every time she had a scan, there was something in the results that required her to go back for further testing.
“Three times I got called back and after the third time, I went on a mission to find out what a preventative mastectomy looks like,” she said.
She consulted with her primary physician, her OB-GYN, a beast surgeon and a plastic surgeon. She asked each doctor what they would do if it was their mother or sister asking them. Each one said they’d recommend getting the mastectomy.
Interestingly, she added, Joanne did not push her to do it.
“Jonie is a scientist and she pointed out that breast cancer is highly treatable and caught early enough, the outlook can be very positive,” Julie said. “But if you talk to women who made this decision, they will tell you that they felt like a ticking time-bomb.”
In early 2022, two years after her hysterectomy, Julie underwent a preventative double mastectomy. It was not an easy decision or an easy recovery, but now that it is over, she is positive she made the right decision.
“I don’t think this is the path for everyone,” she said. “I don’t want to be the poster child for removing body parts to prevent cancer. But that was my decision. I’m grateful that I brought the chances of having breast cancer down and there’s no more screenings. Looking forward I hope for the best, including continuing on with my 47 year old friendship with Jonie!”

