
Deciding what to do after a diagnosis of localized prostate cancer can be difficult. For some slow-growing cancers, active surveillance—closely monitoring the cancer without immediate treatment—may be a safe and effective option.
Read our previous blog on active surveillance vs. treatment.
But when treatment is needed, the main options are surgery or radiation therapy. Both can be very effective, but they come with different potential benefits and risks.
In this post, we’ll take a closer look at how surgery and radiation work, what to expect from each, and how your personal values, daily life, and even your genetics might help you decide what’s best for you.
How Does Surgery (Prostatectomy) Work?
Surgery to remove the prostate is called a radical prostatectomy. The entire prostate is removed, sometimes along with a small amount of surrounding tissue, which can affect the muscles that control urination and the nerves involved in an erection.
There are two main approaches to performing a radical prostatectomy:
- Traditional open surgery: A surgeon makes a single large incision in the abdomen to access and remove the prostate.
- Laparoscopic surgery: A surgeon makes several small incisions in the abdomen and uses special instruments, often with the assistance of a camera, to perform the surgery with minimal invasion.
How Does Radiation Therapy Work?
Radiation therapy treats prostate cancer by using focused energy to kill cancer cells. There are two main types:
- Brachytherapy, which places radiation sources directly inside of the prostate.
- External beam radiation therapy (EBRT), which directs radiation at the prostate from outside the body.
While both types are effective, this post focuses on EBRT, a common option for localized prostate cancer.
Instead of delivering the full dose of radiation all at once, EBRT breaks treatment into smaller doses—called fractions, or “fractionation”—spread out over time.
There are three common ways EBRT can be fractionated:1
- Stereotactic body radiation therapy (SBRT): 5–7 high-dose sessions over 5–10 days.
- Moderately hypofractionated radiation therapy (MHFRT): 20–28 moderate-dose sessions over 4–5 weeks.
- Conventionally fractionated radiation therapy (CFRT): 35–45 low/moderate-dose sessions over 8–10 weeks.
Understanding the basics of surgery and radiation is just the start—next, let’s look at how cutting-edge technology is reshaping these treatments.
How Innovation Is Improving Prostate Cancer Treatment
Prostate cancer treatment has advanced significantly. Modern tools and advanced imaging now make surgery and radiation more precise, less invasive, and easier to recover from.
Advanced Prostatectomy Technologies
- Robotic-assisted prostatectomy: Delivers greater control and 3D visualization through robotic systems, allowing for smaller incisions, less bleeding, and quicker healing.
- Enhanced imaging: Employs real-time tools like ultrasound or fluorescence to help surgeons see and protect critical structures more clearly.
- Nerve-sparing techniques: Uses advanced tools to preserve the nerves that control erections and urination to reduce the risk of long-term side effects.
Advanced Radiation Technologies
- Robotic-assisted radiation: Uses robotic systems like Cyberknife to closely monitor the prostate during treatment, delivering focused radiation that adapts to movement and spares healthy tissue.
- Enhanced imaging: Utilizes advanced real-time imaging and surface-guided systems to target radiation more precisely to the prostate while protecting healthy tissue.
- Protective devices: Involves protective spacers as a temporary barrier between the prostate and rectum to reduce radiation exposure to the bowel and lower side effects.
These advances have improved outcomes and quality of life, empowering you to make a treatment choice that best fits your needs and lifestyle.
But how do these two treatment options compare with one another?
Surgery vs. Radiation
When it comes to localized prostate cancer, both surgery and radiation are equally and highly effective treatments. In fact, a large long-term study published in 2023 found that, after 15 years, survival rates were nearly identical—about 97%—regardless of which treatment patients chose.2
This means the decision isn’t about which option works better to cure the cancer—it’s about understanding how each treatment may affect your body, your recovery, your peace of mind, and your quality of life.
Let’s take a closer look at how they compare.
Initial Risks
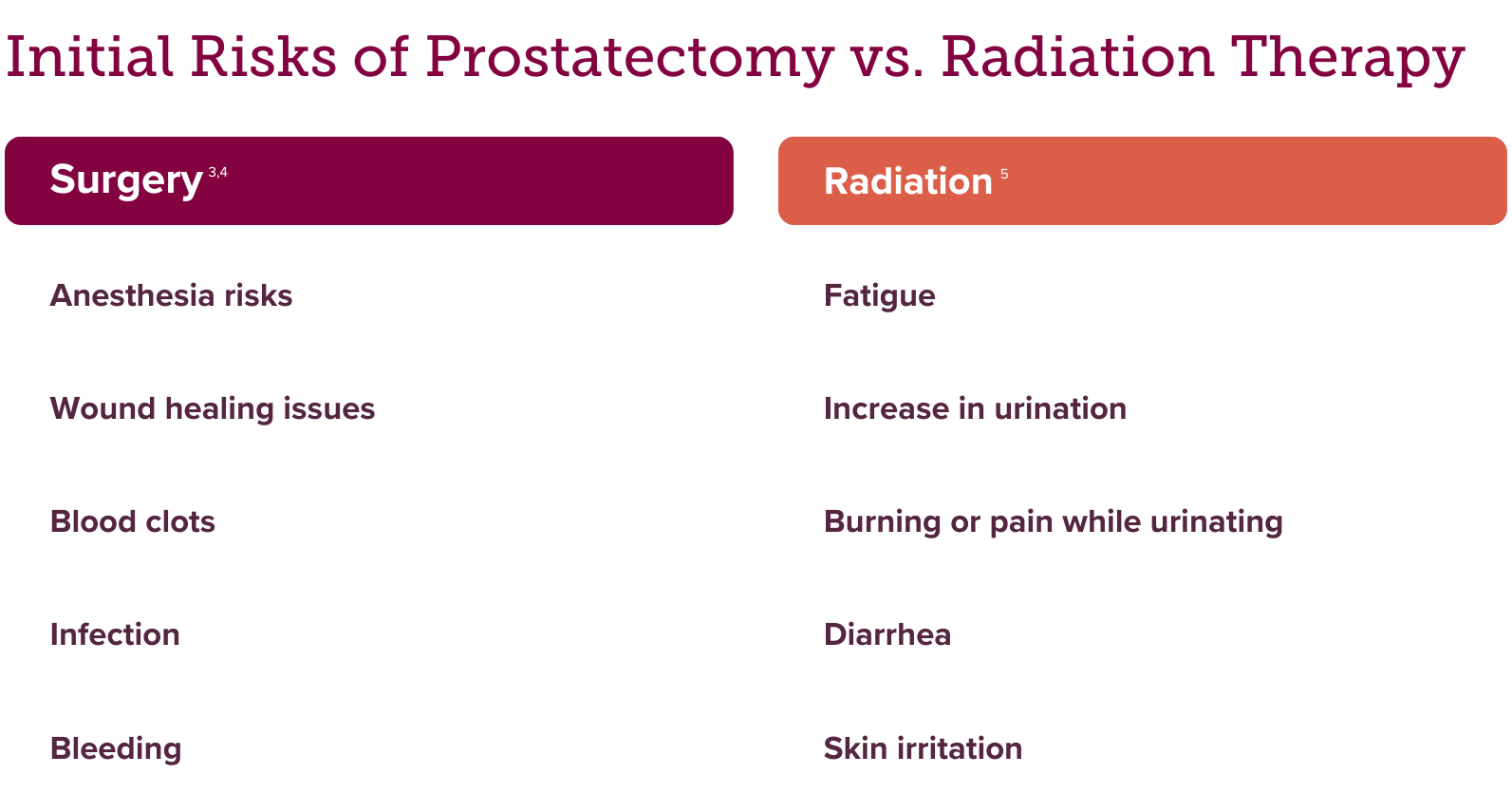
Prostatectomy is a surgery, and like any major operation, it comes with the typical risks associated with anesthesia, surgery, and recovery. Radiation therapy also has its own risks, though they are generally less immediate and severe than those from surgery.
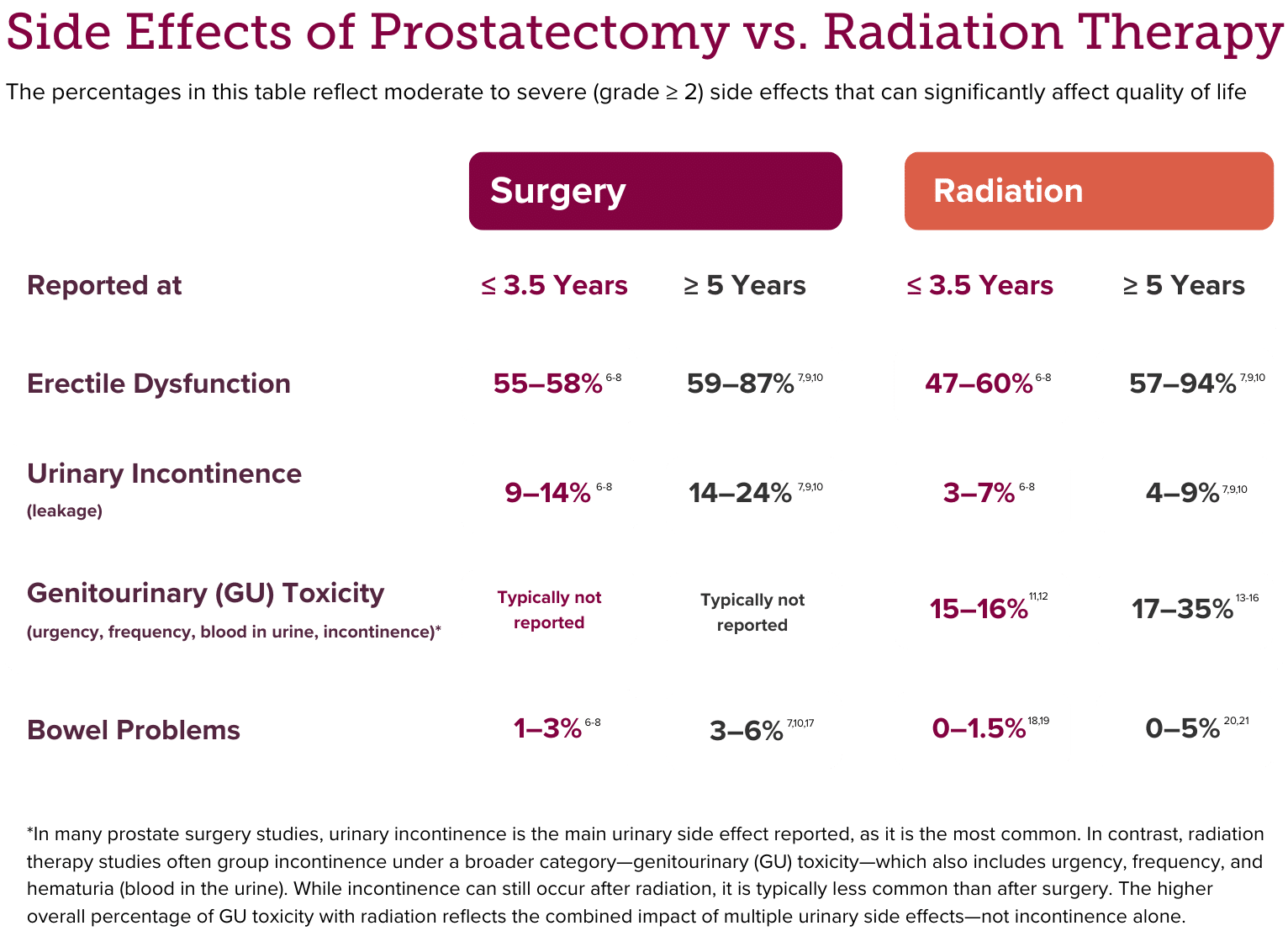
Side Effects
Both treatment options can cause side effects, especially related to sexual, bladder, and bowel function. Comparing these side effects can be difficult because studies differ in how they evaluate, measure, and report them—and everyone’s experience can vary widely. That said, some common patterns have emerged that can let you know what to expect.
Recovery
Recovery from surgery typically takes longer, with several weeks of healing and time away from normal activities. Radiation is delivered over time but has a milder short-term impact, allowing most people to stay active and continue daily routines during treatment.
Peace of Mind
Some people feel more confident with surgery, which removes the cancer and provides a detailed report on how advanced it was. Others prefer radiation because it’s less invasive and doesn’t require a hospital stay.
Quality of Life
The main differences in quality of life usually stem from urinary side effects. Some people struggle more with incontinence after surgery, while others find that radiation-related urinary side effects have a bigger impact. Thinking about what matters most to you in daily life can help guide your decision.
But what if you could know your personal risk of developing urinary side effects from radiation—before starting treatment?
Thanks to advances in genetics, the PROSTOXTM tests now make that possible.
The Role of Genetics in Decision-Making
PROSTOX are genetic tests that analyze specific markers related to how your body responds to radiation. These tests predict your individual risk of developing significant late urinary side effects, known as genitourinary (GU) toxicity, based on the type of radiation therapy you might receive.22-24 In fact, patients with a high-risk PROSTOX score have been shown to be 10 times more likely to develop these side effects than those with a low-risk score.24
There are two PROSTOX tests, tailored to different radiation regimens:
- PROSTOX ultra: for stereotactic body radiation therapy (SBRT); high doses over a short period of time
- PROSTOX CFRT+: for both conventional fractionated radiation therapy (CFRT) and moderately hypofractionated radiation therapy (MHFRT); lower doses over a longer period of time
Since each PROSTOX test analyzes different genetic markers, your risk varies by radiation type. Most patients are low-risk for at least one radiation approach, and fewer than 2% are high-risk for both. So, most people have a radiation option that fits their biology.
While the PROSTOX tests do not make the treatment decision for you, they can give you and your care team personalized insight—so you can confidently choose a plan that not only treats your cancer but also supports your quality of life.
Choosing the Best Prostate Cancer Treatment for You
Surgery and radiation are both often excellent options for treating localized prostate cancer. The best choice depends on your specific diagnosis, how your body may respond, and what matters most to you in life after treatment.
If you’re uncertain, ask your doctor whether a test like PROSTOX could offer more clarity. Personalized tools like this are helping patients make smarter, more confident decisions—so you can move forward with peace of mind.
References
- https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/external-beam
- https://www.nejm.org/doi/full/10.1056/NEJMoa2214122.
- https://my.clevelandclinic.org/health/treatments/24294-prostatectomy#risks-benefits
- https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.prostate-cancer-should-i-have-radiation-or-surgery-for-localized-prostate-cancer.tc1702#
- https://www.cancer.org/cancer/types/prostate-cancer/treating/radiation-therapy.html
- https://jamanetwork.com/journals/jama/fullarticle/2612618
- https://www.nejm.org/doi/full/10.1056/nejmoa1209978
- https://www.nejm.org/doi/full/10.1056/NEJMoa074311
- https://evidence.nejm.org/doi/full/10.1056/EVIDoa2300018
- https://jamanetwork.com/journals/jama/fullarticle/2814131
- https://www.sciencedirect.com/science/article/pii/S2331518024000301
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8979583/
- https://link.springer.com/article/10.1007/s00345-025-05532-5
- https://www.nature.com/articles/s41391-022-00520-x
- https://www.redjournal.org/article/S0360-3016%2820%2933612-9/fulltext
- https://www.thegreenjournal.com/article/S0167-8140(20)30218-8/abstract
- https://evidence.nejm.org/doi/full/10.1056/EVIDoa2300018
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767246
- https://ro-journal.biomedcentral.com/articles/10.1186/s13014-022-02103-5
- https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-12692-x
- https://pubmed.ncbi.nlm.nih.gov/28871986/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8979583/
- https://ascopubs.org/doi/10.1200/JCO.2020.38.6_suppl.163
- https://aacrjournals.org/clincancerres/article/31/12/2530/762786/Validation-and-Derivation-of-miRNA-Based-Germline




Leave a Reply